Learn More
Knee, Common Knee Procedures

Dr. Kimball has been working with a new technology for knee replacement. It offers unique advantages when compared to a traditional knee replacement.
The differences include:
- Patient specific size. Traditional knees have included a limited number of size choices (usually 6) from which surgeons choose. The ConforMis total knee is designed from a CT scan of your knee and thus fits you and only you.
- Patient specific design. The curvatures and shape of traditional knees have evolved from data collected from many knees and represent “averages” of many. The ConforMis knee design is, in many respects, a replica of your knee. It, from the CT scan data, replicates the shape and curvatures that are present in your knee.
- The load-bearing characteristics of a patient specific knee more closely replicates your normal knee and thus has a much larger load bearing area than traditional total knees.
- The ConforMis total knee retains your Posterior Cruciate ligament rather than sacrificing this ligament as is done in PS Stabilized traditional total knees.
- The bone resections required in the ConforMIs total knee are very small when compared to traditional total knees. It is extremely “bone sparing”.
- The position of the components is the result of computer navigation techniques applies to your “pre-operative” CT scan and thus traditional alignments guides which include inserting a rod inside the femur are not necessary. This usually results in diminished blood loss.
- Because the knee is size and design specific to you and because it is ligament and bone sparing the expectations are that it will recover faster, move easier and “feel” more like a normal knee. As with any new design modifications there are no long term outcome studies to prove that this is indeed the case.
Who is a candidate for a patient specific total knee replacement?
Why is a CT scan needed prior to surgery?
Why does it take so long to get a patient specific knee?
Will ConforMis total knee last as long as a more traditional total knee?
- The ConforMis knee is made out of the same materials as almost every other total knee on the market today
- The design of the ConforMis knee is such that the weight bearing area in the knee is more “normal” that a conventional total knee. We expect that, because the weight bearing area is larger, that the knee will actually last longer however there is no long term data to support that opinion at present.
- We assume that if the load bearing is more normal and the movement characteristics for the knee is more normal that it will function better and last longer however we, as yet, have no long term data to support that thesis.
For Dr. Kimball’s full description and explanation packet about ACL Surgery, click here.
Recent reports indicate that surgeons who, on average, do 10 ACL surgeries per year do almost 90% of ACL reconstructions done in America. I perform 120 to 150 ACL reconstructions per year.
Approximately 60% of my ACL’s are done using Patellar Tendon Autografts (because of the number of high demand athletes I treat), another 20% are performed with Hamstring Autografts (Double Bundle Anatomic technique) and the remaining 20% are performed with Allografts usually in a “revision” setting.
ACL Reconstruction (Anterior Cruciate Ligament)
When the ACL tears, in most cases, it explodes. That is why many people feel a “snap” or a “pop” at the moment of injury. As such, the ligament is not repairable and must be “Reconstructed”. In brief, the doctor must make a “New” ligament using some other tissue or “Graft”. There are three (3) common choices of tissue which can be used as a Graft to reconstruct your ACL. Each choice has it’s pros and cons. Below is a summary of the issues involved in Graft selection.
When reconstructing an ACL one must decide what type of tissue to use to fabricate a new ligament. Biologic grafts can be either native tissue (autografts) or acquired cadaver tissue (allografts). Experience with prosthetic or artificial ligaments has led to failures.
Autografts:
Patellar tendon, quadriceps tendon, and semitendinosus/gracilis bundled tendons are the primary autografts in use.
- Patellar tendons grafts are still the gold standard in high demand athletes and have the advantages of bone-to-bone fixation, at both ends, high ultimate tensile strength and high graft stiffness. When this graft heals to bone, the tendinous portion is essentially anchored at both ends. Multi-stranded grafts require healing of all strands to achieve their potential. Patellar tendon grafts may allow slightly earlier return to sport.
As I treat a large number of high level athletes at the professional and college level, I pattern my graft selection after the patterns used on NFL players.
NFL Team Orthopedic surgeons opinions on reconstructing the ACL on an NFL player:
– 100% of those surgeons preferred patellar tendon auto grafts, in a recent survey
– 0% preferred hamstring grafts
– 0% preferred Achilles allograft (cadaver graft)
Patellar Tendon (BTB) (Autologous)
Pros: This graft has high tensile strength, high stiffness of the tissues and allows early bone-to-bone healing at both ends of the graft. Some studies have suggested a higher incidence of residual pain at the donor site however other studies have concluded this not to be the case.
This is the most common graft selected when treating high level, high contact athletes at professional, college and other levels.
Cons: I discourage the use of this graft if the patient spends a lot of time on his/her knees such as occurs in plumbers, tile setters, carpet layers etc. The scar at the donor site is right in the front of the knee may be annoying and uncomfortable in that situation.
Semitendinosus/gracilis bundled tendons (Hamstring)
Pros: This graft is made up by harvesting your semitendinosus and gracilis tendons (hamstring tendons), weaving them into a rope like structure and then implanting that “rope” into the knee in place of the ruptured ACL. It is a strong graft but since it is made up of multiple strands its ultimate strength is dependent on healing of all the strings with exactly the same tension on each strand. Cosmetically this graft is more pleasing as the scar is not directly in the center front of the knee.
Cons: Healing of the tendon strands to the bone occurs at a slightly slower rate than with a bone-to-bone graft. Since the tendons of two muscles are removed, atrophy of muscle in the back of the thigh will occur. This can lead to weakness and cosmetic deformity. This graft also tends to loosen a bit over time and may have a higher failure rate in high demand athletes.
Allograft (Cadaver graft):
Multiple allograft choices have become popular, particularly in the revision setting. These include bone-patellar tendon-bone, quadriceps tendon, hamstring tendon, Achilles tendon, and both anterior and posterior tibialis tendons.
Pros: The advantages of allograft use are less surgical time, less surgical morbidity, faster rehabilitation, and flexibility in graft preparation. The disadvantages include the risk of viral and/or bacterial infection, slower incorporation of allograft tissue, immunologic reactions, and a paucity of long-term outcome data. Cadaver grafts are also more expensive than using your own tissue.
Cons: Since cadaver material comes from a donor, the material must be carefully tested to avoid disease transmission. I have a very long track record with quality providers such that the risk of infection from donor material is actually less than the risk of infection normally associated with any type of surgery.
In reality, hundreds of thousands of various types of allografts are used safely in the U.S. each year. Although there is risk, the risk is very small.
I recommend:
- My approach is to use your own tissue if at all possible. If not, then an allograft can be a good choice.
- Recent studies show that Allograft outcomes are very similar to Patellar Tendon Autografts if a non-irradiated graft is used.
Anatomic or Double Bundle ACL Reconstructive Surgery:
Recent advances in understanding of the complex function and anatomy of the ACL has reaffirmed the importance of performing ACL reconstruction in a fashion which most accurately restores not only the function but to the degree possible, the actual anatomy of the injured ligament.
The normal ACL is made up of two major bundles:
- anterior medial (AM)
- posterior lateral (PL)
The AM bundle contributes primarily to control translation of the knee in flexion. The PL bundle, on the other hand, contributes more to controlling rotational stability as the knee approaches full extension.
Traditional ACL reconstruction techniques applied to high demand athletes (such as foot ball players, soccer players and other athletes which involve high torque exposure) has been done employing a large single bundle graft centered as nearly possible at the anatomic sites of attachment on the tibia and femur. Graft choices primarily include:
- Patellar Tendon Auto-graft (BTB)
- Hamstring Auto-graft (HS)
- Variety of Allograft (Cadaver)
The selected graft is attached to the femur and tibia by implanting the ends of the graft in bone tunnels created at or near the anatomic site of attachment of the normal (uninjured) ligament on the femur and the tibia.
There are a myriad of factors to consider when selecting type of graft to be used as well as the method of fixation of the graft to the bone. As with most choices in life, each has its advantages and disadvantages.
Recent improved understanding of the unique anatomy of the ACL has led surgeons around the world to develop methods of reconstructing the ACL in a more anatomic fashion than has been traditionally employed. This “anatomic” method is also referred to as the “double bundle” method as it employs two smaller bundles (or grafts) rather than one large “single bundle” (graft).
When performing ACL reconstruction with Hamstring Autograft or Hamstring Allograft, I employ double bundle technique.
The “anatomic” method has not been in use for very long and thus we have limited experience with the results of this method especially on high demand athletes. However, early results are certainly promising and the rationale behind the method certainly makes sense.
When performing Patellar Tendon (BTB Autograft) or Cadaver (Allograft) reconstructions I position the graft in the anatomic position.
Summary:
The goal of treatment is to provide a painless knee with stability and normal muscle function and coordination. The challenge is to perform the reconstructive procedure with high success and minimal morbidity. To accomplish this requires a combination of a skilled surgeon, appropriate graft selection and careful attention to the details of rehabilitation. In my experience, a highly motivated patient is almost as important as having a skilled surgeon.
Diagnostic Arthroscopy:
Small incisions (approximately 4 mm) are made in the front of the knee joint. An arthroscope is introduced into the joint. The joint is infused with a physiologic solution. The joint and all structures are examined visually employing a video system. The arthroscope is a small tube with internal fiberoptic light and is attached to a video camera which directs the inside of your knee joint onto a video screen. Dr. Kimball routinely takes a series of still photographs of the findings in your knee such that he can demonstrate to you what he found and what he did. He can usually provide you with your own copy of photographs and will do so at your first post operative office visit.
Dr. Kimball looks the joint surfaces, the tracking of the patella, the medial and lateral meniscus and the anterior (ACL) and posterior (PCL) cruciate ligaments.
Upon completion of the diagnostic portion of the procedure, Dr.Kimball is prepared to proceed with repair and or reconstruction of the damaged structures.
The treatment of cartilage (joint surface) injuries is frequently an important part of the treatment of knee injuries. Often serious knee injuries (torn ACL) are associated with injuries to the joint surface. The management of these injuries require that the surgeon become a BIOSURGEON. This involves the application of treatments and surgical techniques that promote healing or regeneration of the injured joint surface.
There are many treatment options. It is the surgeon who decides which technique to apply to a given joint surface injury.
- Lavage and Debridement
This is a very limited process consisting of cleaning, smoothing or shaving an injured or damaged joint surface.
Pro: Removes debris, spurs and rough spots on the joint surface which can, to a limited degree, reduce some of the mechanical symptoms of “catching”, “locking” or “giving out”.
Con: This procedure does not promote “healing” or “regeneration” of the surface injury. If improvement occurs it is usually short lived and does not significantly alter the course of the underlying disease.
Applications: May have limited use in treating either a minimal joint surface injury or in temporarily reducing mechanical symptoms in a severely injured joint surface. - Drilling and/or Abrasion Arthroplasty
This technique involves araiding the exposed bone in order to stimulate healing and regeneration of tissue. This technique has largely been replaced by “Microfracture” technique described below. - Microfracture (Mesenchymal Stem Cell Stimulation)
This procedure is often applied to relatively small, localized joint surface lesions. This is an arthroscopic procedure and consists of scraping or trimming away the loose, damaged cartilage, lightly scraping the surface from the exposed bone, then creating holes in the exposed bone approximately 2-3 mm. apart. This creates a rough surface for the ensuing blood clot with undifferentiated mesenchymal cells (stem cells) from the marrow to adhere. In other words, a blood clot derived from the bone marrow, fills the defect in the articular surface. If all goes well, this clot will become a “fibrocartilage” patch which fills the defect in the joint surface. Most patients are significantly improved by this procedure.
Pro: Relatively easy to perform. Response and recovery is quite predictable
Con: It is important to protect the healing tissue. This means crutches with only “toe-touch” weight bearing for 6 weeks. It is also important to do passive range of motion several hours per day or apply 1500 unloaded cycles of range of motion per day.
Applications: Used to treat relatively small full thickness cartilage injuries in the under 50 age group. - Osteochondral Grafts
Some lesions are too large to respond favorably to microfracture procedure. In these situations the injured surface may be “replaced” by transporting cartilage “plugs” from one site (less important) in the knee to another (the site of the painful lesion). These “plugs” or in some cases larger pieces of bone and cartilage can be transported from the same knee (your knee). These are called Autografts. Or they may be obtained from an organ donor. These grafts are called Allografts.
When a small graft or grafts will suffice, they are obtained from a less important part of the injured knee. When a very large defect must be treated, the graft must come from a “donor”. Allografts are obtained from Tissue Banks.
- Autografts:
Pro: Can effectively heal relatively large full thickness cartilage lesions. Not associated with risk of rejection from donor material. Not exposed to risk of disease transmission from organ donor.
Con: Size of treatable lesion is limited by need to harvest donor material from another part of the same knee. Thus amount of transportable graft material is limited.
Application: Treatment of relatively large full thickness cartilage lesions. - Allografts:
Pro: Can be used to treat large lesions. No limitations on size or amount of graft material.
Con: Requires implanting biologic material from organ donor thus there is risk of disease transmission from donor, risk of infection from tissue bank processing and risk of rejection from immunologic reaction.
Application: Treatment of very large full thickness cartilage and bone lesions.
Autologous Chondrocyte Implantation (ACI)
This is a very special type of Autograft. Cartilage cells are harvested (via arthroscope), sent to a special lab where the cells are cultured to increase their numbers, then the cells are implanted using a very special technique. This enables one to “regrow” cartilage tissue and fill the defect.
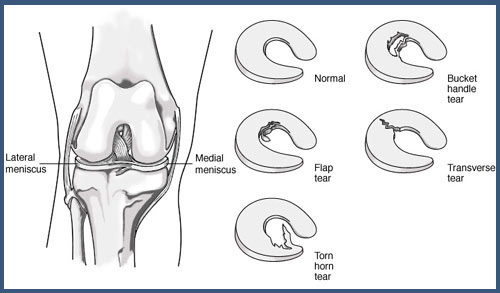
This is one of the more minor arthroscopic knee surgeries. Your procedure is designed to remove the torn part of your meniscus. The goal is, through 3 small puncture wounds, to enter the knee with an arthroscope, visualize what is wrong employing a television monitor then, using very small instruments, remove the damaged part of the meniscus. The procedure usually takes less than 30 minutes.
I have performed this operation thousands of times. You can expect to go home with a slight limp, be sore then next day and then gradually improve. I expect that you will be walking near normally within one week and back to full activity within one month.
Most patients do not require formal physical therapy following this procedure. Most do not require crutches.
The risks associated with this procedure are similar to any operation. We worry about infection, anesthetic complications, medication reactions and blood clots following surgery.
For more information see section dealing with potential complications following surgery.
In some cases it is more appropriate to repair the torn meniscus rather than remove the torn part. This decision is determined by the nature, location and type of tear that is encountered. Some areas of the meniscus have adequate blood supply and have the ability to heal if repaired. Other areas are without sufficient blood supply and thus do not have the ability to heal. The “red zone” is the term we use to describe the areas that have potential for healing. The “white zone” does not have the ability to heal.
When I repair your meniscus I will either suture (sew) it back together or repair it using a special biodegradable “tack” to hold it together while the healing occurs. Healing takes time and I will usually require that you use crutches 3 to 4 weeks following a meniscus repair and limit your return to vigorous activities for 3 to 4 months. Even if we do everything right, you meniscus may not heal and it may be necessary to come back at a later date and re-scope the knee and remove the part that did not heal.
I am more likely to repair a torn meniscus in a younger person as the impact of saving the meniscus will have greater importance.
Partial Knee replacement (Unicompartmental Knee Replacement)
What is a partial knee replacement?
Knee replacements can be classified in several ways. One way is according to the portion of the knee replaced. For example one portion can be replaced (unicompartmental), or two (bicompartmental) or three (tricompartmental). Therefore a unicompartmental knee replacement is a resurfacing or replacement of one compartment of the knee. It is just one of the surgical options for the treatment of osteoarthritis of the knee.
History/Background: The idea of replacing one portion of the knee is not a new concept. It has been studied and performed since the 1970’s. Though it developed at the same time as total knee replacement, the procedure has taken time to gain widespread acceptance in the orthopedic community. This was in part due to early reports of poor results after the procedure. However, further review of these studies shows that those poor results may be attributed to patient selection, the type of artificial component used, and the surgical technique. Identification and correction of pitfalls in the technique, plus the development of better implant designs, have renewed enthusiasm for unicompartmental replacement in certain selected patients. The addition of Computer Navigation to precisely place the components has added significantly to this technically demanding operation.
What are the indications for Unicompartmental Knee Replacement? Every person’s case is different so you should discuss what is right for you with your orthopedic surgeon. But here are the general indications that I use for patients who undergo unicompartmental replacement:
- Pain with weight bearing on one side of the knee (the inside or medial side of the knee.)
- X-ray showing narrowing at predominately one side of the joint.
- Failure to respond to non-operative care or operative efforts at cartilage treatment (repair, replacement, or regeneration of articular cartilage.)
- Frequently Asked Questions-FAQ
For more information on the specific implants Dr. Kimball uses, click here.
Relative Contraindications for the Procedure:
- Inflammatory arthritis like rheumatoid arthritis, lupus arthritis, psoriatic arthritis, arthritis inflammatory bowel disease.
- Severe curvatures of the legs like severe bowleg or knock-knee. Mal-alignment can usually be corrected when total knee replacement is performed, however little if any alignment correction can be obtained when performing partial knee replacement.
- Obesity: Results of partial knee replacement in the obese is less predictable.
After Surgery
After surgery you will receive pain medication and begin physical therapy. It is important to start moving your new knee as soon as possible after surgery to promote blood flow, to regain knee motion, and to facilitate the recovery process. You should be out of bed and walking with crutches or a walker within 24 hours of your surgery.
You will be shown how to safely climb and descend stairs, how to get into and out of a seated position, and how to care for your knee once you return home. It is a good idea to enlist the help of friends or family to help you once you do return home.
Before you leave the hospital, your therapist will show you a variety of exercises designed to help you regain mobility and strength in your knee. You should be able to perform these exercises on your own at home. When at home, it is very important to continue with your exercises as instructed.
The typical recovery from partial knee replacement is much faster than total knee replacement. Many patients go home after an overnight stay. Some may even go home on the day of surgery. Expect to aggressively attack your rehabilitation with the help of a physical therapist and, if possible, a supportive family member who can be with you during the physical therapy on the day of surgery and the next morning if you spend the night.
For Dr. Kimball’s full description and explanation packet about Total Knee Replacement Surgery: click here.
Dr. Kimball Performs Total Knee Replacement Surgery using state of the art technology.
Dr. Kirt Kimball is well known on the Sports page. This year marks his 19th year as Team Orthopedic Surgeon to the BYU Athletic department. His practice is focused on knee and shoulder conditions with special consideration for the needs of high performance athletes. Dr. Kimball performs many Total and Partial knee replacements. Many of his patients are in the “slightly aging athlete” category and as such need knee replacements which will tolerate higher than usual demands. For most of us, once and athlete, always an athlete thus it is important that, if you need your knee replaced, that it be a High Performance knee that will enable the longest wear without failure. The precision alignment of artificial knee components is important for long term wear.
Total Knee Replacement (Total Knee Arthroplasty- TKA): surgery is done to replace the damaged joint with artificial surfaces. Even under the best of circumstances surgery cannot return the joint to its normal state. However, an artificial joint will likely diminish pain and improve functionality.
Timing of the surgery:
“When should I have my knee replaced?” This is a common question and the answer is patient- specific. It varies from patient to patient and is based on a number of variables.
- Do it when the symptoms from your knee no longer adequately respond to less aggressive treatments.
- Do it when the pain sufficiently disrupts your daily living and the worth outweighs the expense, difficulty, and risk necessary to have your knee replaced.
Patients often ask if the “x-ray” says I need a knee replacement? My response is that I don’t treat x-rays but rather “treat people”. The appearance of an x-ray often doesn’t not correlate with the degree of pain, disability or disruption of your quality of life. Consider doing the surgery when your quality of life is disrupted to the degree that you are motivated to move forward.
Sometimes, even in the presence of minimal pain, it is appropriate to do a knee replacement because a deformity is rapidly progressing, or range of motion is deteriorating. This is something we can discuss together so that you can make the best-informed decision.
With few exceptions, I tell patients that they should have the surgery when they are ready. I generally will not tell patients to do it or when to do it, but rather wait for them to tell me that they want to proceed. I also like to emphasize that I “don’t take care of x-rays; but rather, I take care of ‘patients’”. Sometimes x-rays indicate the need for knee replacement but the patient’s symptoms are insufficient to warrant such intervention.
Component selection:
There are several companies that manufacture the hardware used in a Total Knee Replacement. There are a number of variables to consider:
- Surgeons tend to prefer one or two systems based on their experience and personal preference.
- Even though systems have similarities, the choice of which system to use is a critical one.
- Systems vary in their ability to accommodate for size differences, alignment challenges, and stability issues.
- It is difficult for a patient to become completely educated with system options, and therefore, there needs to be a high level of trust between the patient and myself. Ultimately, the components chosen are those best suited for the patient’s situation.
- Some systems are more effective than others in restoring normal “kinematics” of your knee. Kinematics is a way of measuring how your knee moves, bends, and rotates compared to a normal knee.
Knees are available in two basic designs: fixed bearing or rotating platforms.
- In fixed bearing knees, the polyethylene insert is bonded to the tibial (shin bone) component.
- In rotating platforms, a poly insert is allowed to rotate, thus adding another degree of motion and, as some studies indicate, improved long-term wear.
I have extensive experience with “fixed bearing” and “rotating platform” knees. In recent years I have stopped using “rotating platform” knees because, although they have excellent wear characteristics, they are often more difficult to obtain excellent range of motion.
In Europe and Asia, almost equal numbers of Fixed Bearing and Rotating Platform knees are implanted. In the US, fixed bearing has dominated the market because until recently, only J&J/Depuy had FDA approved components. Now most manufactures have FDA approved rotating platform devices.
I primarily use two systems of total knee components in my practice. I most often use a patient specific design manufactured by ConforMis. When a patient specific custom component is not appropriate, I use Medacta (a Swiss made component)
- ConforMis:
- Patient Specific Total Knee
In the past few years I have enjoyed extensive experience with a custom made, patient specific total knee system. I have performed approximately 600 total knees with this technology. It has significant advantages when compared to “off-the-shelf” designs.
ConforMis is presently the only system in the US that manufactures patient specific total knees. All other systems can be classified as “off-the-shelf” designs. Examples of “OTS” knees include Zimmer, Biomet, Stryker, Depuy, Wright Medical, and ODC to name a few.
OTS (Off-the-shelf) knees are manufactured in bulk in a variety of sizes from which the surgeon chooses at the time of surgery. The ConforMis knee is designed from a CT scan of the patient’s knee. The CT scan is used by the manufacturer to create a component that exactly matches the patient’s knee both with respect to size and, more importantly, the actual shape of the knee. OTS knees have a “generic” shape. Individual knees vary tremendously with respect to size and shape. The ConforMis knee effectively “resurfaces” your existing knee as opposed to replacing it with a generic size and shape.
The ConforMis knee has been demonstrated to produce improved outcomes compared to OTS knees in the following areas:
- Less bone is removed at surgery
- Less bleeding occurs after surgery
- Less pain occurs after surgery
- Recovery is faster
- Range of motion is better
- The knee kinematics more closely matches a normal knee than any other knee on the market.
- As such, there is a higher satisfaction rating by patients after total knee replacement that with OTS knees.
Not all patients are candidates for a ConforMis knee. In those patients I use Medacta. This is an excellent OTS knee manufactured in Switzerland.
When is a patient NOT a candidate for a Patient Specific Knee?
Severe deformity
Severe bone loss
Severe loss of motion
Severe ligamentous instability
The ConforMis knee is analogous to a “resurfacing procedure”. Some knees are so badly destroyed that resurfacing is inadequate in restoring function. In those situations I employ Medacta technology. In my practice approximately 90% of the knees I treat are good candidates for ConforMis technology.
Computer Navigation Technology:
I was one of the first surgeons in the US to routinely employ Computer Navigation in total knee replacement in the operating room. This enhanced my ability to properly align the total knee. The technology was expensive, added time to the operative procedure, but was an important improvement. With ConforMis knees, the CT scan is employed to correct alignment using Navigation technology however; it is done in the manufacturing process by creating patient specific cutting jigs along with the patient specific components. This enables the advantages of Navigation however that portion of the procedure is done prior to going to the Operating room thus reducing cost and time in the OR.
ConforMIS technology uses computer navigation technology in the manufacturing process rather in the Operating room. It uses the pre-operative CT scan of your leg.
Standard instrumentation does not use computer navigation; rather, it relies on external and internal alignment rods and jigs to help assure proper component positioning. Although it is a time proven technique it is not as accurate as Computer Navigation.
Fixation of implant:
Implants are fixed to the bone by using either cemented or non-cemented technique. Cemented technique is clearly the “gold standard” and according to most studies it produces the best long-term results. Sometimes non-cemented methods are appropriate. It requires ‘in’ growth of your bone into the implant to assure solid fixation. Although slightly less reliable than cemented technique, it can also produce good results.
Pain Control Protocol, Medications, and Hospital Stay
Pain Control:
For several years I have been using what is referred to as a “multimodal” approach to pain management. It recognizes that there are various pain receptor sites in the brain and if we block those sites before we cause pain, the effect is much better than if we cause the pain and then try to ‘catch up’ with medication. Therefore, about an hour before the surgery we administer three different types of oral pain medications. We continue those for several days after the surgery to maintain the “blockade” of the receptor sites in the brain. Studies and experience has proven that this results in far superior pain relief.
Pre-Operative Medications:
If there are medications that you have already been taking from home (home medications), we will discuss them at your pre operative appointment. There may be some that you need to stop taking before surgery.
There are three basic types of receptor sites in the brain responsible for the transmission of pain. Each receptor type can be blocked with a specific medication. It is known that if we block the receptor site before the pain stimulus occurs, the result of reduced pain is far superior to that which occurs if the blockade is not started until after the pain stimulus happens. Again, approximately one hour prior to surgery, three separate oral medications are administered.
- A narcotic (usually a small dose of a long acting morphine derivative)
- Acetaminophen (Tylenol)
- A Cox 2 analgesic (usually Celebrex)
All three of these medications are continued in relatively low doses throughout the hospital stay and for the first week or two after hospital discharge in order to keep the receptor sites constantly blocked.
Anesthesia at time of Surgery:
I prefer, and almost require, regional anesthesia instead of general anesthesia, for total and partial knee replacement. Regional anesthesia means a spinal anesthetic combined with gentle sedation and a long acting local anesthetic injected in the tissues around the knee at the time of surgery.
This is superior in many ways—
- You will feel better and not as “drugged” after the surgery.
- You will have less difficulty with nausea following the surgery.
- You will have a much lower risk of blood clots and pulmonary embolism.
- It is reliable and safer than a general anesthetic, in my experience.
What is a spinal anesthetic?
This is an injection of a long acting local anesthetic medication into the spinal fluid in your low back region. It causes numbness and weakness in the legs that can last for up to 24 hours. This is not to be confused with an epidural anesthetic where the numbing medication is placed adjacent to the spinal sack rather than in the spinal sack. In my experience, epidural anesthesia is less reliable.
Intra-Operative Medications:
The anesthesiologist primarily controls medications administered during the course of the surgery. They include the anesthetic agents that are part of the spinal anesthetic, as well as muscle relaxers and tranquilizing medications. Unlike general anesthetic, you are not completely asleep, however, drugs are often administered such that you do not remember any of the details of the experience since you are generally not completely asleep as occurs during a general anesthetic.
Additionally, antibiotic medication is provided to help reduce the risk of infection as well as any other medications that may be useful considering your general medication condition and anesthetic needs.
Post-Operative Medications:
Post-Operative Medications:
When you are ready to go home you will most likely continue with any medications you were taking before you came to the hospital for this surgery. This will be discussed upon discharge.
You will also be given RX for the following:
- Anticoagulation
- Low dose long-acting analgesics (pain relief medication- usually for 7 to 10 days)
- Short acting analgesics to be taken as needed according to a prescribed schedule
- Anti-nausea medication if needed
- Muscle relaxation medication if needed
- Anti-inflammatory medication
Where do I go after hospital discharge?
Most of my total knee patients are discharged from the hospital on the 2nd or 3rd day following surgery. Most go directly home. This assumes that their home environment is sufficient to meet their needs. To go home, one must have sufficient help at home to help you through the first several days. If you think in-home nursing care might be needed then going to a local rehabilitation facility is probably a better choice than going directly home. An attentive spouse or family member is usually sufficient for discharge to home. If you are uncomfortable about your home situation, there are several local rehabilitation facilities that you might consider. My office can share with you our experience and recommendations.
If you go home, a home physical therapist will come to your home for 1-3 weeks and help continue the therapy program you started in the hospital. Not all home physical therapists are the same. We can advise you regarding those with whom we have good experience.
Once you are sufficiently mobile, it may be appropriate to continue your rehabilitation at a local outpatient physical therapy unit or a local gym. These decisions are dictated to a large degree based on your progress, your level of independence and your motivation.
Improved technology and improved outcomes now enable us, in some circumstances, to perform total knee replacement in an outpatient setting. In this situation you spend 23 hours in the outpatient facility and then go home or to a sub-acute skilled nursing facility for a few days. This may dramatically reduce the overall cost of total knee replacement.
Blood loss issues:
With current technology I rarely encounter the need for blood transfusion following total knee replacement. Thus it is NOT my practice to have you donate your own blood in advance, nor expect to have to receive a transfusion from someone else.
Exceptions to this are extremely rare in my experience.
Blood Clot (DVT- deep vein thrombosis) Prophylaxis/ Anticoagulation:
DVT describes the condition when blood clots within a vein, thus obstructing the vein. When the clotted or thrombosed vein is inflamed and painful, one may use the term thrombophlebitis. A DVT is a potentially dangerous condition. If the clot breaks loose from where it formed, it may move to the lungs and cause a pulmonary embolism. A pulmonary embolism can be fatal. A number of things are done both in the hospital and after hospital discharge to minimize the risk of this serious complication. Unfortunately there is no assurance that these treatments will work.
In Hospital:
Treatments done both in and out of the hospital include mechanical measures as well as medicinal measures.
Mechanical Measures:
Some of the following measures MAY be used to attempt to reduce the risk of developing a blood clot:
- Active leg exercises and early return to function. Nothing works better than active muscle contractions in encouraging good circulation.
- Compression of the veins in the legs to minimize pooling of stagnant blood that may lead to clot formation.
- Use of elastic stockings of other devices to compress leg veins.
- Use of elastic wraps or similar devices to compress leg veins.
- Use of mechanical devices that compress veins in the foot and increase circulation. These are often used during surgery of all types to aide blood circulation in your legs even though you may be asleep under a general anesthetic.
- Elevation of legs to facilitate blood return to the heart.
Medicinal Measures:
Depending on your specific “risk” factors, some of the following measures may be used in attempting to reduce the risk of a blood clot during and following your procedure:
- Use of blood thinning medication
- Coumadin
- Heparin or Lovenox or similar medication
- Aspirin
- Use of a filter inserted in the major vein (inferior vena cava) below the heart to catch clots and prevent them from getting to your lungs and causing a pulmonary embolism. This procedure is done by a cardiologist (usually 24 hours prior to the planned surgery).
My Approach to DVT/Pulmonary Embolism Prophylaxis: I prefer to maximize mechanical and medical measures. This means:
- Compression devices on foot/calf.
- Early range of motion and out of bed walking after surgery as soon as possible.
- Use of oral anticoagulant medication is started on the day following surgery.
- Continue oral anticoagulants 7-10 days following hospital discharge. Sometimes we go longer if the risk appears to be higher than normal.
- Unfortunately sometimes we do everything we can and we still experience DVT and Pulmonary Embolism! If that does occur, we attempt to recognize it early and treat it aggressively.
Infection Concerns:
My Approach to preventing infection:
- Delay surgery if there appears to be a source of acute or chronic infection anywhere in your body.
- Start intravenous antibiotics approximately 1 hour prior to the start of surgery.
- Continue intravenous antibiotics 24 hours after the start of surgery.
- Employ strict sterile techniques in the operating room to prepare the operative site and minimize risk of contamination.
- ConforMis technology employs disposable single use instruments rather than instruments that are used over and over by other patients and surgeons. There is evidence that this method further reduces the risk of infection.
- Use surgical techniques that minimize the duration of the surgery. Evidence shows that the longer the operation, the higher the infection rate.
- Monitor patient and surgical wound post operatively to identify and treat early signs of infection.
- Sometimes infection occurs even though everything possible to prevent it was done. Signs of infection should be carefully monitored. If any signs of infection are found, the infection will be treated aggressively.
Physical Therapy
Before Surgery:
Physical therapy and exercise therapy when performed prior to surgery has some limited value. Unfortunately most patients anticipating surgery are in pain, and aggressive exercise often only makes the pain worse. Efforts to improve range of motion prior to surgery are not often effective. Resistive exercises to improve strength are encouraged. Recent studies demonstrate that efforts at physical therapy PRIOR to total knee replacement REDUCE the need for physical therapy after the surgery and improve outcomes.
In Hospital:
Physical therapy and rehabilitation starts on the day of surgery. I prefer that you get out of bed and are at least standing, if not taking a few steps, on the afternoon following surgery. I start active and passive range of motion exercises on the day of surgery and continue through the hospital stay and at home following discharge. I employ CPM, which is a Continuous Passive Motion machine to help you gain range of motion after surgery.
After Discharge from the Hospital:
Home physical therapy is arranged to assist you for the first week or two following hospital discharge. It consists primarily of doing much of the same exercises that you started in the hospital. It will include use of the CPM as well as therapist directed exercises. Your specific need for these services will vary with your own difficulties and motivation. As soon as you are able to successfully continue on your own or in an outpatient facility home physical therapy can be discontinued.
Outpatient therapy is sometimes needed as an adjunct to home physical therapy. This involves going to a local facility and receiving instruction and assistance in gaining range of motion, strength and endurance. We can assist you in selecting a physical therapist with expertise in total knee rehabilitation.
After undergoing Total Knee Replacement: These are some of the important directions to
be aware of:
Dr. Kirt Kimball Total Knee Discharge Instructions
The following discharge instructions are from specific from Dr. Kimball. These instructions are general guidelines. Your individual needs may vary depending on your condition. Please contact Dr. Kimball’s office for more information if needed.
Blood Clot Prevention:
You have been prescribed a medication (Aspirin, Eliquis, Xeralto, Lovenox, or Warfarin) to help
reduce your risk of getting a blood clot. It is important you take this as prescribed for the
duration of the prescription. Along with taking your other medication, movement is one of the best ways to prevent blood clots. Continue to do ankle pumps while laying and sitting. Walk every 1-2 hours throughout the day, while awake.
Signs of a blood clot:
- Swelling in thigh, calf, or ankle that does not decrease with elevation.
- Pain, warmth, and tenderness in calf, back of knee or groin area.
- Blood clots can form in either leg.
- If you have any of these symptoms, please reach out to your surgeon.
- Shortness of breath or chest pain could represent a pulmonary embolism. This is a blood clot that moved to your lung and represents an emergency (911).
Managing Pain, Discomfort, and Side Effects:
You are going to experience a fair amount of pain. You have been prescribed medication to help in the management of pain and inflammation. Getting pain relief will help you rest better and do important exercises so your new joint will heal properly. Follow the instructions on the
prescription label and track the use of your pain medication in a log. It is important to remember to take pain medication before activity and bedtime. When your pain has been controlled, you may slowly decrease the amount of medication you are taking (such as – taking one tablet instead of two; or increase the time between doses). Narcotics should be the first medication you taper off. Only take the medications prescribed in addition to your regular medications for other medical conditions (ie. Hypertension/diabetes/etc) If your medication is not effectively managing your pain, please try:
- Applying ice to your incision or painful areas
- Lying flat and elevating your leg above your heart
- Changing your position frequently
- Using distraction, try doing things you enjoy– reading, watching TV, or listening to music
DO NOT drive or consume alcoholic beverages while on narcotics.
Pain Medication Refills: keep track of pain medication quantity. You must give the office 24-
hour advanced notice before you will run out of medication. Make sure to plan ahead, especially for weekends and holidays, as it is difficult for your surgeon to prescribe medications after hours. Have your medication and pharmacy information ready when you call. Current State Law severely restricts all physician’s ability to prescribe pain medication in an attempt to curtail opioid addiction. Although well-intended, these restrictions sometimes make it difficult to take care of patient’s needs.
Constipation is a common side effect of opioid pain medication. Continue taking stool softeners and follow the Step by Step Bowel Care Guide for After Surgery. It is a great resource to help prevent or manage constipation. If you have not had a bowel movement
within 7 days, please contact your surgeon. Stop stool softeners if you begin to have loose stool or diarrhea.
Nausea can be a side effect of pain medication. Make sure to eat something before taking
pain medications to help decrease the risk of nausea. If you are experiencing nausea, start refueling your body by drinking small amounts of clear liquids such as 100% fruit juice or broths. Bland carbohydrates are easy to digest and will typically not aggravate the stomach
when you are feeling nauseated. Carbohydrate options include crackers, bread, bananas, applesauce, or Jell-O. It is my routine to prescribe an anti-nausea medication in anticipation of
this possibility.
Mild dizziness is a common side effect of pain medication. Be careful as you walk or climb stairs. Notify your surgeon if the dizziness persists and it is keeping you from walking and being
active.
Breathing deeply will help prevent a respiratory infection following surgery. Take deep
breaths every hour until you are back to your usual level of activity. If you were sent home with an Incentive Spirometer, use it 10 times each hour while you are awake and you follow up with your surgeon.
Incision Care:
Knee Surgery
Your incision will be covered with a waterproof dressing and covered with an ACE elastic bandage when you go home. You may remove the ACE elastic wrap 24 hours after your surgery to shower. It’s okay to let water and soap run across the waterproof dressing. Rinse clean and
pat dry. Rewrap leg with ACE elastic bandage to help with compression. No lotions, ointments or creams, should be placed on or around the surgical site or dressing. No soaking or submerging in water such as hot tubs, bathtubs, swimming pools, for 4-6 weeks or until the
wound is completely healed and no scabs are present.
You can expect to have some redness and warmth around the incision site and swelling extending above and below the joint. Bruising and discoloration around your operation site is normal.
Change your dressing if the edges become loose and water seeps into it while showering. Some drainage is normal and can be expected. If your dressing becomes saturated and there are multiple large dark spots migrating to the edges of the dressing, then you need to change your dressing. Using the ACE bandage for compression can help slow the bleeding and drainage. The drainage should slow down and stop within 24-48 hours. If the drainage persists, or you notice a significant increase in redness or warmth, please call your surgeon’s office immediately. In most cases, your original waterproof dressing is still in place when you see Dr. Kimball at your
first post op office visit.
Swelling:
Swelling is to be expected after a joint replacement. It can cause increased pain and limit your range of motion. Swelling is best controlled by following the R.I.C.E. Method:
REST – Getting enough rest will help your body heal and reduce swelling.
ICE – It is recommended to apply ice for 20-30 minutes every 1-2 hours, after physical
therapy/activity, and before you go to bed. Ice can help to reduce and minimize the internal scarring process. Always make sure there is something between your skin and the ice to help prevent an ice burn. Place ice packs on the outside of your clothes, or place ice packs inside of a
clean pillowcase or dishtowel before applying it to your joint.
Compression – Using an elastic bandage or compression stockings keeps extra fluid from collecting in and around your joints. You will be using an ACE wrap to help dress your knee incision. This will help with swelling. This should be snug but not too tight. The ACE wrap should be changed daily in order to check your skin and can be hand washed with a mild detergent and hung up to dry if it becomes soiled.
Elevate – Several times a day, elevate your leg ABOVE the level of your heart. You may use pillows to elevate the leg. Place the pillows long ways starting just below the knee going towards your heel. If you are doing your exercises to stretch the knee flat, it is ok if a pillow is placed under your knee for limited amount of time.
Diet:
Eating high quality sources of protein will aid in wound healing and help to prevent muscle loss during the recovery process. Examples of quality protein: cottage cheese, yogurt, beans/lentils, salmon, chicken or other lean meats, eggs, and nuts/nut butters. Eating fruits, vegetables, nuts, and whole grains will help prevent constipation. Drinking plenty of fluids will keep you well hydrated and help to prevent constipation. Forte Post Op (Forteelements.com) is an excellent source for the nutritional elements needed to facilitate recovery. Otherwise protein supplements, Vitamin C, Lysine, Vitamin D and a multivitamin have been shown to facilitate recovery.
Activity:
Your physical therapist has created an exercise plan to strengthen and retrain your muscles as you get used to using your new joint.. A consistent effort is important. Avoid overdoing it in any single therapy session. Assistive devices (walker, crutches) are mandatory until your strength and balance have returned and you are no longer limping. You will be scheduled to begin Out Patient physical therapy within a few days following your surgery. In some cases, a home health nurse and physical therapist may come to your home during the first week following surgery.
Frequent, short walks are the key to a successful recovery. It is recommended that you stand and move around every 1-2 hours during the waking hours of the day. Increase your activity gradually. A balance between activity and rest is necessary.
You may have difficulty sleeping at night due to discomfort in the operative extremity. Getting up and moving can help to alleviate the discomfort. Problems sleeping are usually not due to a sleep disorder and sleeping medication is usually not appropriate. More effective pain management should lead to better sleep. As an alternative, Tylenol PM is a safe sleeping aid.
Please call Dr. Kimball at 801-373-7350 for any of the following:
*There is an answering service available 24/7, 365 days a year. A medical team member will return your call.
- Pain that gets worse or cannot be controlled with prescribed medications.
- Problems with your incision – Unusual bleeding, new drainage, blood, pus, foul odor, or separation of the incision edges.
- A fever > 101.5 that doesn’t get better after taking your medication.
- No bowel movement within 7 days.
- Nausea or vomiting and unable to keep food and fluids down.
- Signs of deep vein thrombosis (blood clot) – pain, excessive swelling, warmth, or redness in the back of the calf.
Call your Primary Care Physician for any of the following:
- Questions regarding your regular medications such as blood pressure, diabetic, or heart medications.
- Symptoms of a urinary tract infection or difficulty urinating.
- Trouble controlling your blood sugar (if you have diabetes).
RETURN to ER for the following:
- Chest pain
- Difficulty breathing – shortness of breath
- Black or bloody stool
- Vomiting blood
- Signs and symptoms of a stroke
Questions or concerns:
During business hours, you can contact the Total Joint Nurse Coordinator:
Melanie Johnson, BSN, RN Office: 801.357-2447 Cell: 385-312-7946
For Rx refills or appointments please call Dr. Kimball’s assistant at 801 373-7350 during regular business hours.
After Business Hours: For after hour emergencies, call 801-373-7350 and the answering service will page the provider on call.
Long-Term Issues
Why do total knees fail?
- Implant design: Some systems seem to wear better than others.
- Surgical Technique: If your surgeon puts in the knee in less than ideal alignment it is more likely to fail early.
- Postoperative rehabilitation and compliance: As the patient, you play an important role in the immediate and long-term success of your surgery. Knee surgery is harder to recover from than hip surgery. You must be ready to work very hard post-operatively, or you will likely not be happy with your result.
What about infection?
It is known that patients with joint replacements who are having invasive procedures performed or who have other infections are at increased risk of the infection spreading to their prosthetic joint. Antibiotic prophylaxis may be considered for those patients who are at risk. Most recent recommendations are that antibiotics be employed on the day of the procedure for such things as dental work and other more invasive procedures. This should be done for at least the first two years following implantation of your new joint. Some believe that it should be done indefinitely. I will discuss with you the best approach for your particular situation.
Wear and implant Failure:
How long will a total knee last?
There are a number of factors that contribute to the answer.
- Some knee systems have better long-term experience than others.
- Many off the shelf total knees done, 20 years ago using technology that we no longer use, have demonstrated survivals in the 90% range at 20 years. Based on current science we believe the technology we are currently using will exceed the results obtained in the past.
- To assure the longest wear it is important that the device be properly aligned and that your use is reasonable and appropriate.
- I am often asked if it is permissible to run, ski, jump, etc. on a replaced knee. The answer is not known. There are no good studies addressing the impact of high energy sports on the survival of knee replacements. Most patients are happy to have a knee that doesn’t hurt and works well for normal daily activities. One company has recently started marketing an “ all terrain” knee. The implication, though not stated, is that somehow this knee will better handle aggressive activity. Some also market a “sports total knee”. I am sorry to admit that there is NO DATA to support these claims. These statements, in my opinion, are marketing claims and wishful thinking.
The Most Common Reasons why total knees fail and require revision:
- Infection
- Loosening
- Instability
- Patellofemoral complications
- Polyethylene wear
Minimally Invasive Total Knee Replacement:
Recently there have been attempts to do this operation through a smaller incision. Many surgeons use a 10-12 inch incision. My standard incision is approximately 6 inches; however the opening varies with the size of the patient. It is possible to do the surgery through a 3 ½ inch incision. Recent studies however, have shown there is a high complication rate, higher incidence of poor component alignment, and no significant advantage to the patient. Some sill advocate this approach. However, experience has taught that I can produce a more reliable result through a 6-inch incision. This is a decision I believe should be left to the surgeon. The fact that your incision is a couple of inches shorter will offer little pleasure if your knee fails prematurely, or does not work as anticipated.
Small incisions (approximately 4 mm) are made in the front of the knee joint. An arthroscope is introduced into the joint. The joint is infused with a physiologic solution. The joint and all structures are examined visually employing a video system. The arthroscope is a small tube with internal fiberoptic light and is attached to a video camera which directs the inside of your knee joint onto a video screen. Dr. Kimball routinely takes a series of still photographs of the findings in your knee such that he can demonstrate to you what he found and what he did. He can usually provide you with your own copy of photographs and will do so at your first post operative office visit.
Dr. Kimball looks the joint surfaces, the tracking of the patella, the medial and lateral meniscus and the anterior (ACL) and posterior (PCL) cruciate ligaments.
Upon completion of the diagnostic portion of the procedure, Dr.Kimball is prepared to proceed with repair and or reconstruction of the damaged structures.
